Substance Abuse & Addiction Disorders
Neurofeedback has emerged as a promising therapeutic intervention for individuals grappling with substance use disorder (SUD) and addiction. Unlike traditional medication approaches, which often target symptoms or cravings, neurofeedback focuses on the underlying neural dysregulation that contributes to addictive behaviors. Substance use disorders are complex, involving alterations in neural pathways related to reward, motivation, and self-control. Neurofeedback aims to address these dysregulations by training individuals to self-regulate their brain activity.
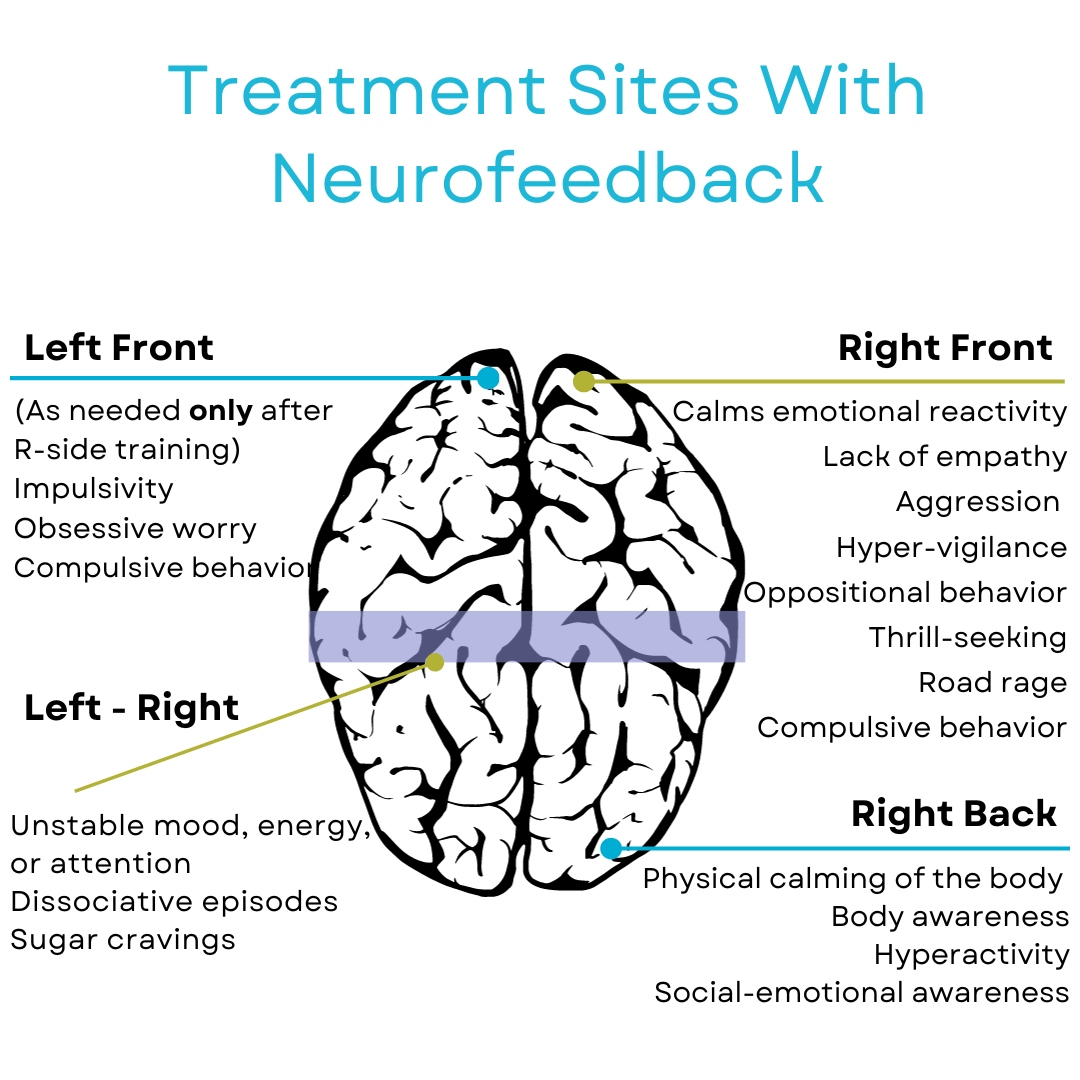
One of the advantages of neurofeedback in treating addiction is its individualized approach. Treatment protocols can be tailored to target specific brain regions affected by substance use, promoting neuroplasticity and aiding in the restoration of healthier neural patterns. This stands in contrast to medication, which may have a more generalized impact on brain function without addressing the personalized nature of addiction-related neural changes.
Research has indicated that neurofeedback can be effective in reducing cravings, improving impulse control, and enhancing emotional regulation in individuals with substance use disorders. By providing real-time information about brain activity and reinforcing positive neural patterns, neurofeedback equips individuals with the tools to better self-regulate and manage the challenges associated with addiction.The lasting impact of neurofeedback is particularly crucial in addiction treatment, where sustained recovery is the ultimate goal.
Studies
deBeus, R. J. (2007). Quantitative electroencephalography-guided versus Scott/Peniston neurofeedback with substance abuse outpatients: A pilot study. Applied Psychophysiology and Biofeedback, 35(4), 146-151. For the past thirty years, electroencephalographic (EEG) biofeedback has been employed in treating substance use disorders (SUD). These disorders, characterized by a complex range often accompanied by various coexisting conditions and diverse EEG abnormalities, have seen potential improvements through the integration of EEG biofeedback with other therapeutic approaches. Clinical studies, guided by efficacy criteria endorsed by the Association for Applied Psychophysiology and Biofeedback and the International Society for Neurofeedback and Research, highlight alpha-theta training as a potentially effective intervention. This training shows promise independently for alcoholism or combined with beta training for stimulant and mixed substance abuse. Notably, when integrated into residential treatment programs, alpha-theta training exhibits potential for positive outcomes. The discussion also touches upon considerations for future research design, taking these factors into account, and provides insights into ongoing research in this domain.
Dehghani-Arani F, Rostami R & Nadali H. (2013). Neurofeedback training for opiate addiction: improvement of mental health and craving. Appl Psychophysiol Biofeedback. 2013 Jun;38(2):133-41. doi: 10.1007/s10484-013-9218-5. Neurofeedback treatment has shown psychological benefits in individuals with substance use disorders, yet its acceptance for substance dependence remains limited. This study aimed to evaluate neurofeedback’s effectiveness for opiate dependence disorder. In an experimental study with 20 opiate-dependent patients, the experimental group received 30 neurofeedback sessions alongside their regular maintenance treatment, while the control group continued with standard care. Results indicated improvements in mental health, including somatic symptoms and depression, as well as positive changes in opioid cravings for the experimental group compared to the control group. These findings support neurofeedback as a supplemental therapeutic approach for opiate dependence disorder.
Harlé KM, Simmons AN, Norman SB, Spadoni AD. Neural affective mechanisms associated with treatment responsiveness in veterans with PTSD and comorbid alcohol use disorder. Psychiatry Res Neuroimaging. 2020 Aug 20;305:111172. Post-traumatic stress disorder (PTSD) often involves neuro-physiological abnormalities linked to heightened anticipatory anxiety and reactivity to trauma-related cues. The effectiveness of PTSD treatment is associated with neural mechanisms, particularly the hyperactivation of the affective salience network. However, it’s uncertain whether these mechanisms extend to individuals with comorbid PTSD and alcohol use disorder (AUD). In a study involving 31 Veterans with both conditions, participants were randomly assigned to prolonged exposure or non-exposure-based treatment. Using fMRI, they underwent an affective anticipation task before and after treatment. Results showed that a greater reduction in PTSD symptoms was linked to decreased anticipatory activation in the right pre-Supplementary Motor Area (pre-SMA), associated with emotion regulation. Conversely, a smaller reduction in PTSD severity was associated with increased anticipatory activation in the right parahippocampal region, linked to affective processing. These findings suggest that targeting post-treatment reductions in anticipatory reactivity in the pre-SMA and para-hippocampal area through neurofeedback training may serve as an alternative or enhancement to other PTSD treatment modalities for individuals with co-occurring PTSD and AUD.