Concussions & TBI's
Concussions and Traumatic Brain Injuries (TBIs) are common occurrences resulting from blunt force trauma or a violent jolt to the head. Concussions, often referred to as mild TBIs, involve a temporary disruption of normal brain function, while more severe TBIs can lead to lasting cognitive and neurological impairment. Both conditions can manifest with symptoms such as headaches, dizziness, memory problems, and mood disturbances, underscoring the need for effective interventions to alleviate these debilitating effects.
Neurofeedback emerges as a promising and non-invasive approach to mitigating the symptoms of Concussions and TBIs. It offers a holistic perspective by addressing not only the immediate symptoms but also the underlying dysregulation in neural activity. By enhancing self-regulation and promoting healthier neural patterns, neurofeedback has the potential to contribute to long-term recovery and resilience against recurring symptoms. Additionally, the non-invasiveness and lack of side effects associated with neurofeedback make it an attractive option, especially in cases where individuals may be averse to or unable to tolerate certain medications.
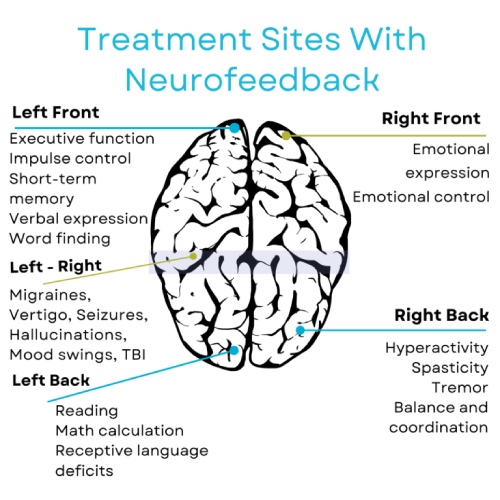
Protocols can be tailored to target regions affected by the injury, facilitating neuroplasticity and encouraging the brain to self-correct. This targeted approach contrasts with medication, which may have a more generalized impact on brain function.
Neurofeedback stands out as a promising therapeutic modality for reducing the symptoms of concussions and TBIs. Its personalized and adaptive nature, coupled with its focus on addressing the underlying neural dysregulation, positions neurofeedback as a valuable complement or alternative to traditional medication in the management of these traumatic brain injuries.
Studies
Ianof, J. N., & Anghinah, R. (2017). Traumatic brain injury: An EEG point of view. Dementia & neuropsychologia, 11(1), 3–5. https://doi.org/10.1590/1980-57642016dn11-010002. Traumatic brain injury (TBI) is a silent epidemic. Mild traumatic brain injury (mTBI) causes brain injury that results in electrophysiologic abnormalities visible on electroencephalography (EEG) recordings. The purpose of this brief review was to discuss the importance of EEG findings in traumatic brain injury. Relevant articles published during the 1996-2016 period were retrieved from Medline (PubMed). The keywords were in English and included “traumatic brain injury”, “EEG” and “quantitative EEG”. We found 460 articles, analyzed 52 and selected 13 articles. EEG after TBI shows slowing of the posterior dominant rhythm and increased diffuse theta slowing, which may revert to normal within hours or may clear more slowly over many weeks. There are no clear EEG or quantitative EEG (qEEG) features unique to mild traumatic brain injury. Although the literature indicates the promise of qEEG in reaching a diagnosis and indicating prognosis of mTBI, further study is needed to corroborate and refine these methods.
Khoury S, Chouchou F, Amzica F, Giguère JF, Denis R, Rouleau GA, Lavigne GJ. (2013). Rapid EEG activity during sleep dominates in mild traumatic brain injury patients with acute pain. J Neurotrauma.2013 Apr 15;30(8):633-41. doi: 10.1089/neu.2012.2519. Epub 2013 Apr 18. Chronic pain is a highly prevalent post-concussion symptom occurring in a majority of patients with mild traumatic brain injury (mTBI). About half of patients with mTBI report sleep-wake disturbances. It is known that pain can alter sleep quality in this population, but the interaction between pain and sleep is not fully understood. This study aimed to identify how pain affects subjective sleep (Pittsburgh Sleep Quality Index [PSQI]), sleep architecture, and quantitative electroencephalographic (qEEG) brain activity after mTBI. Twenty-four mTBI patients complaining of sleep-wake disturbances, with and without pain (8 and 16, respectively), were recruited 45 (±22.7) days post-trauma on average. Data were compared with those of 18 healthy controls (no sleep or pain complaints). The PSQI, sleep architecture, and qEEG activity were analyzed. Pain was assessed using questionnaires and a 100-mm visual analogue scale. Patients with mTBI reported three times poorer sleep quality than controls on the PSQI. Sleep architecture significantly differed between patients with mTBI and controls but was within normal range. Global qEEG showed lower delta (deep sleep) and higher beta and gamma power (arousal) at certain EEG derivations in patients with mTBI compared with controls (p<0.04). Patients with mTBI with pain, however, showed greater increase in rapid EEG frequency bands, mostly during REM sleep, and beta bands in non-REM sleep compared with patients with mTBI without pain and controls (p<0.001). Pain in patients with mTBI was associated with more rapid qEEG activity, mostly during REM sleep, suggesting that pain is associated with poor sleep and is a critical factor in managing post-concussion symptoms.