ADHD & ADD
A significant body of research has been conducted on Attention-Deficit Hyperactivity Disorder (ADHD) and Attention-Deficit Disorder (ADD). With Neurofeedback we have found biomarkers in the brain for attention issues. A Brain Map (QEEG) allows us to see where the frequencies are misaligned. Patients are frequently able to go off of stimulant medications after neurofeedback sessions are employed. Sleep is also regulated, since dysregulated sleep has a significant impact on focus and attention.
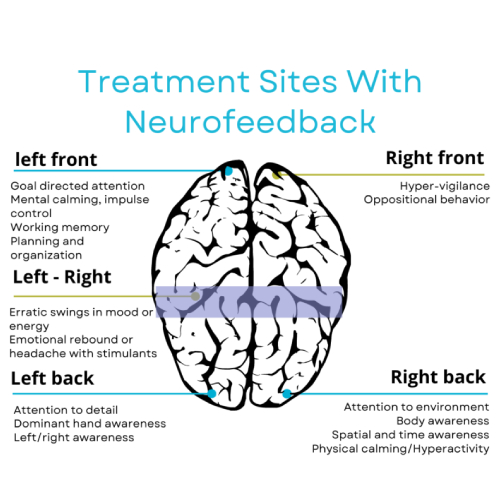
Reducing symptoms of ADHD with Neurofeedback is centered around enhancing specific areas of the brain crucial for attention, executive function, and impulse control—primarily targeting the frontal lobes. Numerous studies in neuroscience have demonstrated that non-pharmaceutical interventions, such as exercise, brain training, specific supplements, and neurofeedback, can effectively enhance frontal lobe functions.
Dr. Kakaiya identifies factors that can naturally improve each patient’s attention and guides patients in making healthier daily choices. The concurrent use of neurofeedback treatment, alongside integrative suggestions, aids in fostering a sense of calmness and increasing focus.
ADHD is a extensively studied domain for Neurofeedback training. Neurofeedback consistently exhibits minimal or no notable side effects and significantly contributes to positive neuropsychological and behavioral outcomes related to ADHD. This involves a decrease in symptoms of inattention and hyperactivity. Other research underscores its ability to improve emotional self-regulation and self-control, effectively addressing issues with overactivity and functional deficits.
Studies
Arns M, Drinkenburg W, Leon Kenemans J. (2012). The effects of QEEG-informed neurofeedback in ADHD: an open-label pilot study. Appl Psychophysiol Biofeedback. 2012 Sep;37(3):171-80. In addressing ADHD, numerous EEG biomarkers have been identified, particularly in connection with the effectiveness of stimulant medication. This pilot study sought to tailor neurofeedback treatment to these specific EEG biomarkers related to ADHD, aiming to enhance clinical outcomes. The objective was to personalize neurofeedback protocols for distinct sub-groups and explore whether this targeted approach could yield improved results. Moreover, the study delved into the neurophysiological effects of neurofeedback by examining pre- and post-treatment EEG and ERP changes in a selected sub-group. Using QEEG-informed neurofeedback, twenty-one ADHD patients underwent treatment, and the impact on inattention (ATT), hyperactivity/impulsivity (HI), and concurrent depressive symptoms was assessed. The results were compelling, indicating a significant enhancement in both inattention, hyperactivity/impulsivity and comorbid depressive symptoms following QEEG-informed neurofeedback. This pilot study stands out as the first to demonstrate the feasibility of selecting neurofeedback protocols based on individual EEG biomarkers, suggesting a notable improvement in treatment outcomes, especially regarding inattention. Nevertheless, it is crucial to note that these findings should be substantiated through further controlled studies. The application of SMR neurofeedback showcased specific changes in ERP and EEG, underscoring the targeted efficacy of this approach.
Arns, M., Feddema, I., & Kenemans, J. L. (2014). Differential effects of theta/beta and SMR neurofeedback in ADHD on sleep onset latency. Frontiers in human neuroscience, 8, 1019. https://doi.org/10.3389/fnhum.2014.01019. Recent research indicates the potential role of sleep and sleep issues in the development of attention deficit hyperactivity disorder (ADHD). A new model suggests that sensori-motor rhythm (SMR) neurofeedback may improve ADHD symptoms like inattention and hyperactivity/impulsivity by normalizing sleep. This study compared 19 adult ADHD patients to 28 controls, examining differences in sleep parameters such as Sleep Onset Latency (SOL), Sleep Duration (DUR), and overall reported sleep problems (PSQI). We also looked into whether there is a connection between these sleep parameters and ADHD symptoms. Additionally, in 37 ADHD patients, we explored the effects of SMR and Theta/Beta (TBR) neurofeedback on ADHD symptoms and sleep parameters. We found a consistent link between self-reported sleep problems (PSQI) and inattention in adults with and without ADHD. TBR neurofeedback showed a slight decrease in SOL, but this change didn’t correlate with the improvement in ADHD symptoms, happening mainly in the latter half of treatment, possibly due to general symptom improvement rather than TBR neurofeedback specifically. On the other hand, SMR neurofeedback notably reduced SOL and PSQI scores. Changes in SOL and PSQI strongly correlated with improvements in inattention, with SOL reduction occurring early in treatment, suggesting it plays a role in the response to SMR neurofeedback. Clinically, both TBR and SMR neurofeedback had similar effects on reducing ADHD symptoms (inattention and hyperactivity/impulsivity), indicating distinct effects and mechanisms in treating ADHD.
Arnold, L. E., Lofthouse, N., Hersch, S., Pan, X., Hurt, E., Bates, B., Kassouf, K., Moone, S., & Grantier, C. (2013). EEG neurofeedback for ADHD: double-blind sham-controlled randomized pilot feasibility trial. Journal of attention disorders, 17(5), 410–419. https://doi.org/10.1177/1087054712446173. Objective: This pilot trial examined the feasibility of a double-blind, sham-controlled design for neurofeedback (NF) in ADHD, and compared the effectiveness of two versus three treatments per week. Method: Unmedicated 6- to 12-year-olds with DSM-IV ADHD were randomly assigned to active NF or sham-NF, and to either 2X or 3X weekly treatment. Results: Over two school years, 39 participants were enrolled with 34 (87%) completing all 40 treatments. Guesses about treatment assignment were no better than chance. At Treatment 24, 38% chose 2X weekly and 62% chose 3X weekly. Both active NF and sham showed significant improvement in parent ratings, with no significant difference between the two. Conclusion: Blinding was effective, with no hindrance to recruitment or retention by the sham. Treatment 3X per week was preferred and equally effective compared to 2X per week. A large double-blind RCT is both feasible and necessary to further assess NF effectiveness for ADHD.